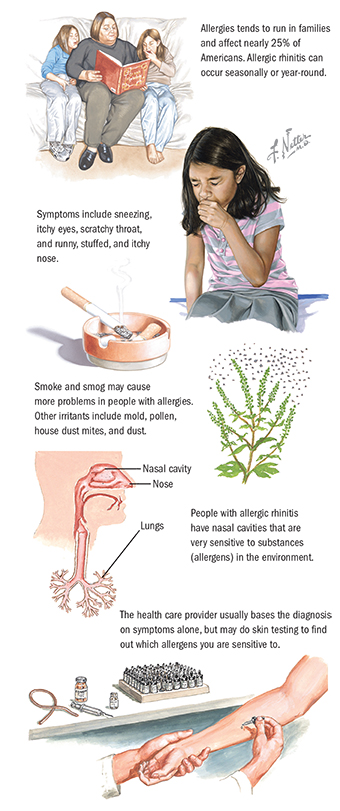
Allergic rhinitis consists of symptoms that occur after exposure to certain substances. This reaction is called an allergy. Allergies can be seasonal (hay fever), especially in spring and fall for a sensitivity to tree and grass pollens. Allergies can also occur year-round (e.g., to pets or house dust mites). Having allergies tends to run in families. Allergies usually occur in people younger than 20 but can develop at any age.
Allergic rhinitis is not contagious and can be controlled.
Irritants include smoke, smog, pollens, molds, and dust.
The most common symptoms include sneezing, itchy eyes, scratchy throat, and runny, stuffed, and itchy nose. Other symptoms are headaches and pressure in the front of the face, and difficulty sleeping.
Long-term problems assocated with allergic rhinitis are nasal polyps (growths in the nose) and loss of the sense of smell.
The health care provider usually uses symptoms alone for diagnosis. The health care provider may in some cases do skin tests to see which substances cause the symptoms. In people with chronic cough, a lung function test may help rule out asthma.
The best treatment usually involves reducing or avoiding exposure to substances causing symptoms (allergens), along with using antihistamines, and nasal decongestants. Preventing symptoms with drugs and using a mask in areas of high exposure to allergens may also help. People who respond poorly to drugs may get shots (injections, called desensitization or immunotherapy). These injections of an allergen are given in increasing doses to get the body to block the allergic reaction. Immunotherapy can now also be administered in the form of medication that dissolves when placed under the tongue (sublingual administration). Possible drug side effects of medications used to treat allergies include sleepiness (oral antihistamines), palpitations or changes in blood pressure (oral decongestants), and thinning of tissues in the nose (intranasal steroids).
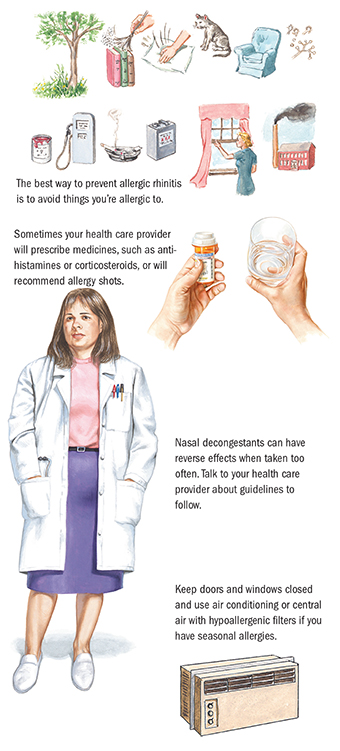
Treatment by an allergist (a doctor trained in treating allergies) or an ear, nose, and throat specialist may be needed in severe or resistant cases.
Contact the following sources:
Copyright © 2016 by Saunders, an imprint of Elsevier, Inc.
Ferri’s Netter Patient Advisor